Book Your Appointment
Deep vein thrombosis (DVT)
Get At Swasthyam Superspeciality Hospital
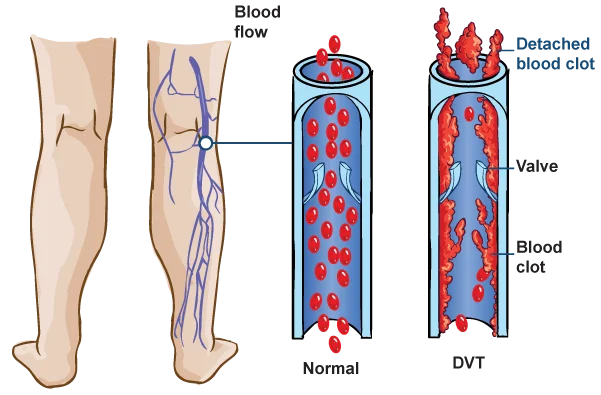
Deep vein thrombosis (DVT) occurs when a blood clot (thrombus) forms in one or more of the deep veins in your body, usually in your legs. Deep vein thrombosis can cause leg pain or swelling but also can occur with no symptoms.
You can get DVT if you have certain medical conditions that affect how your blood clots. A blood clot in your legs can also happen if you don’t move for a long time, such as after you have surgery or an accident, when you’re traveling a long distance, or when you’re on bed rest.
Deep vein thrombosis can be very serious because blood clots in your veins can break loose, travel through your bloodstream and get stuck in your lungs, blocking blood flow (pulmonary embolism). However, pulmonary embolism can occur with no evidence of DVT.
When DVT and pulmonary embolism occur together, it’s called venous thromboembolism (VTE).
Symptoms?
DVT signs and symptoms can include:
- Swelling in the affected leg. Rarely, there’s swelling in both legs.
- Pain in your leg. The pain often starts in your calf and can feel like cramping or soreness.
- Red or discolored skin on the leg.
- A feeling of warmth in the affected leg.
-
Deep vein thrombosis can occur without noticeable symptoms.
Causes
Anything that prevents your blood from flowing or clotting normally can cause a blood clot.
The main causes of DVT are damage to a vein from surgery or trauma and inflammation due to infection or injury.
Causes
Anything that prevents your blood from flowing or clotting normally can cause a blood clot.
The main causes of DVT are damage to a vein from surgery or trauma and inflammation due to infection or injury.
Risk factors
Many things can increase your risk of developing DVT. The more risk factors you have, the greater your risk of DVT. Risk factors for DVT include:
- Age. Being older than 60 increases your risk of DVT, though it can occur at any age.
- Sitting for long periods of time, such as when driving or flying. When your legs remain still for hours, your calf muscles don’t contract. Muscle contractions normally help blood circulate.
- Prolonged bed rest, such as during a long hospital stay, or paralysis. Blood clots can form in the calves of your legs if your calf muscles don’t move for long periods.
- Injury or surgery. Injury to your veins or surgery can increase the risk of blood clots.
- Pregnancy. Pregnancy increases the pressure in the veins in your pelvis and legs. Women with an inherited clotting disorder are especially at risk. The risk of blood clots from pregnancy can continue for up to six weeks after you have your baby.
- Birth control pills (oral contraceptives) or hormone replacement therapy. Both can increase your blood’s ability to clot.
- Being overweight or obese. Being overweight increases the pressure in the veins in your pelvis and legs.
- Smoking. Smoking affects blood clotting and circulation, which can increase your risk of DVT.
- Cancer. Some forms of cancer increase substances in your blood that cause your blood to clot. Some forms of cancer treatment also increase the risk of blood clots.
- Heart failure. This increases your risk of DVT and pulmonary embolism. Because people with heart failure have limited heart and lung function, the symptoms caused by even a small pulmonary embolism are more noticeable.
- Inflammatory bowel disease. Bowel diseases, such as Crohn’s disease or ulcerative colitis, increase the risk of DVT.
- A personal or family history of DVT or PE. If you or someone in your family has had one or both of these, you might be at greater risk of developing DVT.
- Genetics. Some people inherit genetic risk factors or disorders, such as factor V Leiden, that make their blood clot more easily. An inherited disorder on its own might not cause blood clots unless combined with one or more other risk factors.
- No known risk factor. Sometimes, a blood clot in a vein can occur with no apparent underlying risk factor. This is called an unprovoked VTE.
Prevention
Measures to prevent deep vein thrombosis include the following:
- Avoid sitting still. If you have had surgery or have been on bed rest for other reasons, try to get moving as soon as possible. If you’re sitting for a while, don’t cross your legs, which can block blood flow. If you’re traveling a long distance by car, stop every hour or so and walk around.
- Don’t smoke. Smoking increases your risk of getting DVT.
- Exercise and manage your weight. Obesity is a risk factor for DVT. Regular exercise lowers your risk of blood clots, which is especially important for people who sit a lot or travel frequently.
Treatment
There are three main goals to DVT treatment.
- Prevent the clot from getting bigger.
- Prevent the clot from breaking loose and traveling to the lungs.
- Reduce your chances of another DVT.
DVT treatment options include:
Blood thinners. DVT is most commonly treated with anticoagulants, also called blood thinners.
Clot busters. Also called thrombolytics, these drugs might be prescribed if you have a more serious type of DVT or PE, or if other medications aren’t working.
Filters. If you can’t take medicines to thin your blood, you might have a filter inserted into a large vein — the vena cava — in your abdomen.
Compression stockings. These special knee socks reduce the chances that your blood will pool and clot.




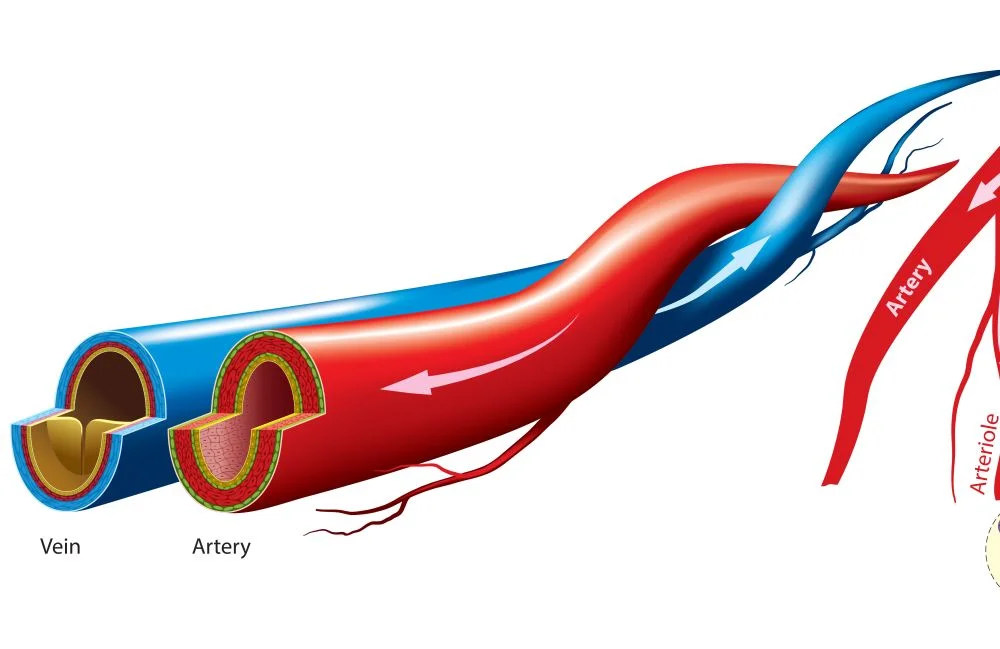
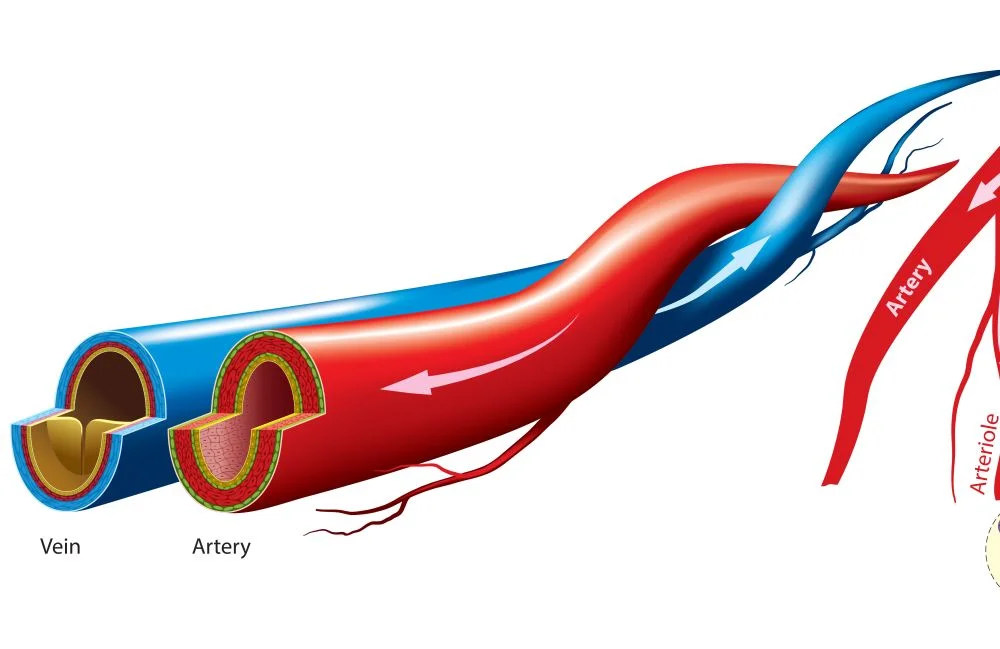
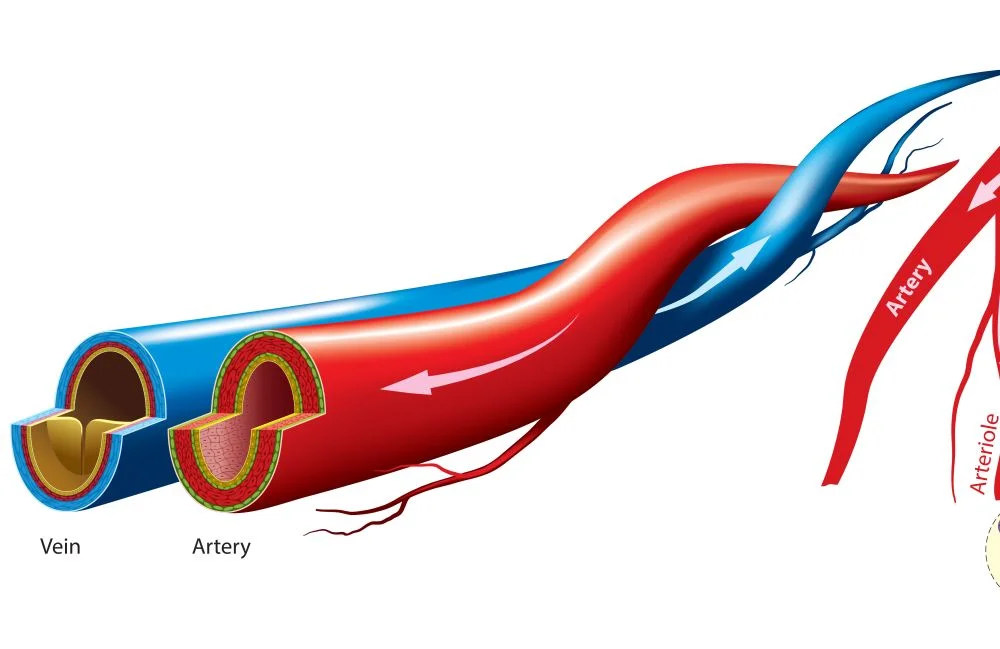
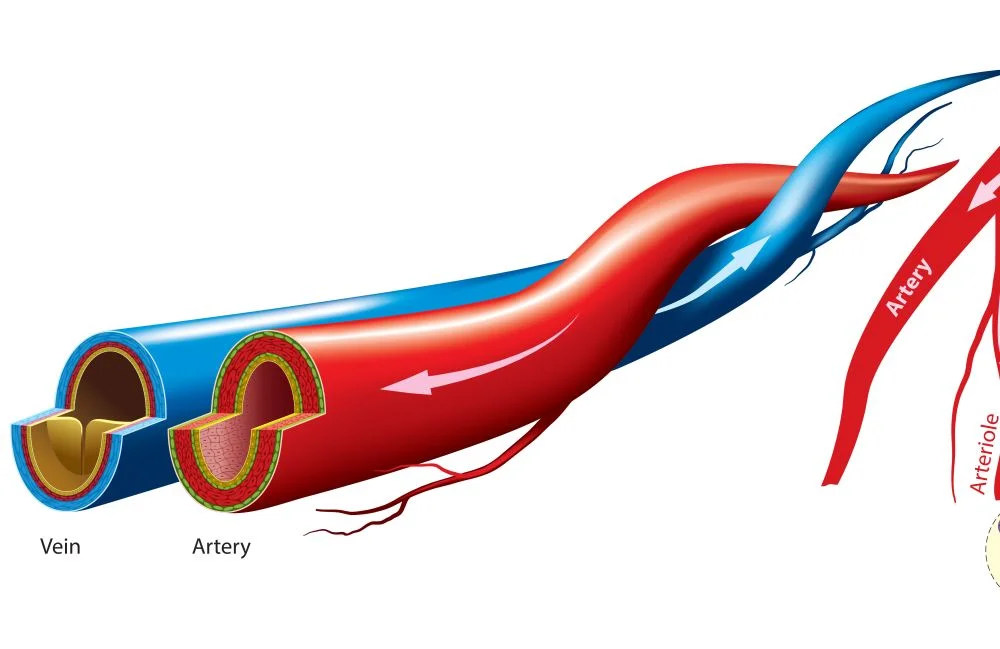
What is a Vascular Surgery?
Vascular surgery is a dynamic and rapidly expanding specialty that deals with comprehensive diagnostic and therapeutic services for patients with diseases and disorders of the arteries, veins, and lymphatics (circulatory system)
Vascular surgeons manage diseases of the veins and arteries in every part of the body except the brain and the heart.
Vascular surgeons are trained in different kinds of procedures
They can perform open, complicated surgery as well as modern minimally invasive endovascular procedures. So they are often known as vascular & endovascular surgeons or vascular specialists. This helps most vascular specialists to give a balanced opinion, unlike other specialists who usually perform only one type of procedure. Therefore, patients can be assured that they will get the best treatment for their particular needs.
Message Us
Get In touch with us. Ask Any Question or Book Your Appointment Now
Emergency
+91-8600888444
Book An Appointment
0712-2222111
Contact Us
Location
97/98 Vivekanand Nagar, Near Sai Mandir, Wardha Road, Nagpur
Contact for
Emergency :- +91-8600888444
Book An Appointment:- 0712-2222111
For Latest Updates Follow Us On Facebook
