Book Your Appointment
Heart Failure
Get Solution At Swasthyam Superspeciality Hospital
Heart Failure
Heart failure, sometimes known as congestive heart failure, occurs when your heart muscle doesn’t pump blood as well as it should. Certain conditions, such as narrowed arteries in your heart (coronary artery disease) or high blood pressure, gradually leave your heart too weak or stiff to fill and pump efficiently.
Not all conditions that lead to heart failure can be reversed, but treatments can improve the signs and symptoms of heart failure and help you live longer. Lifestyle changes — such as exercising, reducing sodium in your diet, managing stress and losing weight — can improve your quality of life.
One way to prevent heart failure is to prevent and control conditions that cause heart failure, such as coronary artery disease, high blood pressure, diabetes or obesity.
Symptoms?
Heart failure can be ongoing (chronic), or your condition may start suddenly (acute).
Heart failure signs and symptoms may include:
- Shortness of breath (dyspnea) when you exert yourself or when you lie down
- Fatigue and weakness
- Swelling (edema) in your legs, ankles and feet
- Rapid or irregular heartbeat
- Reduced ability to exercise
- Persistent cough or wheezing with white or pink blood-tinged phlegm
- Increased need to urinate at night
- Swelling of your abdomen (ascites)
- Very rapid weight gain from fluid retention
- Lack of appetite and nausea
- Difficulty concentrating or decreased alertness
- Sudden, severe shortness of breath and coughing up pink, foamy mucus
- Chest pain if your heart failure is caused by a heart attack
Causes
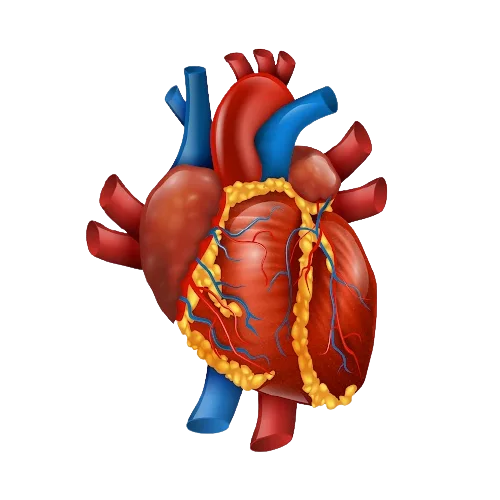
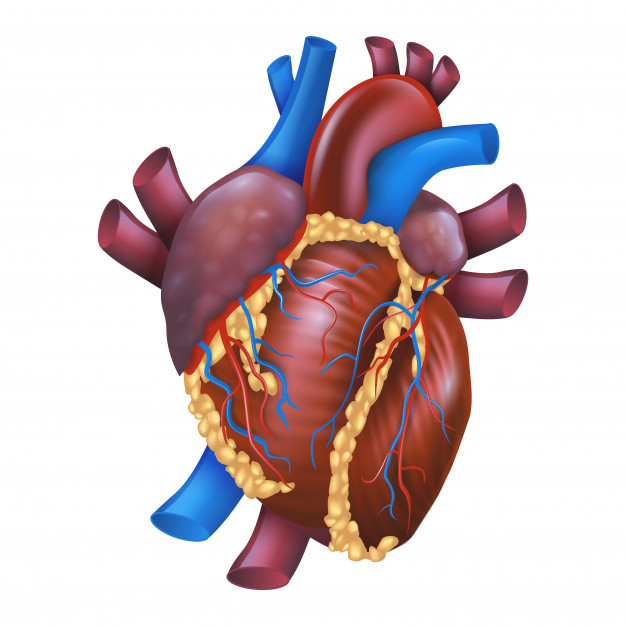
Heart failure often develops after other conditions have damaged or weakened your heart. However, the heart doesn’t need to be weakened to cause heart failure. It can also occur if the heart becomes too stiff.
In heart failure, the main pumping chambers of your heart (the ventricles) may become stiff and not fill properly between beats. In some cases of heart failure, your heart muscle may become damaged and weakened, and the ventricles stretch (dilate) to the point that the heart can’t pump blood efficiently throughout your body.
Over time, the heart can no longer keep up with the normal demands placed on it to pump blood to the rest of your body.
An ejection fraction is an important measurement of how well your heart is pumping and is used to help classify heart failure and guide treatment. In a healthy heart, the ejection fraction is 50 percent or higher — meaning that more than half of the blood that fills the ventricle is pumped out with each beat.
Causes
Heart failure often develops after other conditions have damaged or weakened your heart. However, the heart doesn’t need to be weakened to cause heart failure. It can also occur if the heart becomes too stiff.
In heart failure, the main pumping chambers of your heart (the ventricles) may become stiff and not fill properly between beats. In some cases of heart failure, your heart muscle may become damaged and weakened, and the ventricles stretch (dilate) to the point that the heart can’t pump blood efficiently throughout your body.
Over time, the heart can no longer keep up with the normal demands placed on it to pump blood to the rest of your body.
An ejection fraction is an important measurement of how well your heart is pumping and is used to help classify heart failure and guide treatment. In a healthy heart, the ejection fraction is 50 percent or higher — meaning that more than half of the blood that fills the ventricle is pumped out with each beat.
Risk factors
A single risk factor may be enough to cause heart failure, but a combination of factors also increases your risk.
Risk factors include:
-
High blood pressure. Your heart works harder than it has to if your blood pressure is high.
-
Coronary artery disease. Narrowed arteries may limit your heart’s supply of oxygen-rich blood, resulting in weakened heart muscle.
-
Heart attack. A heart attack is a form of coronary disease that occurs suddenly. Damage to your heart muscle from a heart attack may mean your heart can no longer pump as well as it should.
-
Diabetes. Having diabetes increases your risk of high blood pressure and coronary artery disease.
-
Some diabetes medications. The diabetes drugs rosiglitazone (Avandia) and pioglitazone (Actos) have been found to increase the risk of heart failure in some people. Don’t stop taking these medications on your own, though. If you’re taking them, discuss with your doctor whether you need to make any changes.
-
Certain medications. Some medications may lead to heart failure or heart problems. Medications that may increase the risk of heart problems include nonsteroidal anti-inflammatory drugs (NSAIDs);
Prevention
The key to preventing heart failure is to reduce your risk factors. You can control or eliminate many of the risk factors for heart disease — high blood pressure and coronary artery disease, for example — by making lifestyle changes along with the help of any needed medications.
Lifestyle changes you can make to help prevent heart failure include:
- Not smoking
- Controlling certain conditions, such as high blood pressure and diabetes
- Staying physically active
- Eating healthy foods
- Maintaining a healthy weight
- Reducing and managing stress
Prevention
The key to preventing heart failure is to reduce your risk factors. You can control or eliminate many of the risk factors for heart disease — high blood pressure and coronary artery disease, for example — by making lifestyle changes along with the help of any needed medications.
Lifestyle changes you can make to help prevent heart failure include:
- Not smoking
- Controlling certain conditions, such as high blood pressure and diabetes
- Staying physically active
- Eating healthy foods
- Maintaining a healthy weight
- Reducing and managing stress
Treatment
Heart failure is a chronic disease needing lifelong management. However, with treatment, signs and symptoms of heart failure can improve, and the heart sometimes becomes stronger. Treatment may help you live longer and reduce your chance of dying suddenly.
Doctors usually treat heart failure with a combination of medications. Depending on your symptoms, you might take one or more medications, including:
- Angiotensin-converting enzyme (ACE) inhibitors: These drugs help people with systolic heart failure live longer and feel better. ACE inhibitors are a type of vasodilator, a drug that widens blood vessels to lower blood pressure, improve blood flow and decrease the workload on the heart.
- Angiotensin II receptor blockers: These drugs, which include losartan (Cozaar) and valsartan (Diovan), have many of the same benefits as ACE inhibitors.
- Beta blockers: This class of drugs not only slows your heart rate and reduces blood pressure but also limits or reverses some of the damage to your heart if you have systolic heart failure.These medicines reduce the risk of some abnormal heart rhythms and lessen your chance of dying unexpectedly. Beta blockers may reduce signs and symptoms of heart failure, improve heart function, and help you live longer.
- Diuretics: Often called water pills, diuretics make you urinate more frequently and keep fluid from collecting in your body. Diuretics, such as furosemide (Lasix), also decrease fluid in your lungs so you can breathe more easily.
- Aldosterone antagonists: These drugs include spironolactone (Aldactone) and eplerenone (Inspra). These are potassium-sparing diuretics, which also have additional properties that may help people with severe systolic heart failure live longer.
- Inotropes: These are intravenous medications used in people with severe heart failure in the hospital to improve heart pumping function and maintain blood pressure.
- Digoxin (Lanoxin): This drug, also referred to as digitalis, increases the strength of your heart muscle contractions. It also tends to slow the heartbeat. Digoxin reduces heart failure symptoms in systolic heart failure. It may be more likely to be given to someone with a heart rhythm problem, such as atrial fibrillation.
Message Us
Get In touch with us. Ask Any Question or Book Your Appointment Now
Emergency
+91-8600888444
Book An Appointment
0712-2222111
Contact Us
Location
97/98 Vivekanand Nagar, Near Sai Mandir, Wardha Road, Nagpur
Contact for
Emergency :- +91-8600888444
Book An Appointment:- 0712-2222111
For Latest Updates Follow Us On Facebook
